1. Why Distinguishing Acne from Lupus Matters
Acne vs Lupus
The appearance of red, persistent bumps on the face can be easily dismissed as common acne vulgaris—a frustrating, but generally benign, skin condition. However, for a small but significant number of individuals, these lesions may be a sign of something much more serious: Systemic Lupus Erythematosus (SLE). This presents a critical differential diagnosis challenge for both patients and clinicians.
The Core Difference: Systemic vs. Dermatological
The fundamental difference lies in their cause (etiology):
- Acne Vulgaris is a localized dermatological disorder primarily affecting the pilosebaceous unit. It stems from the overactivity of sebaceous glands and inflammation within the skin.
- Systemic Lupus Erythematosus (SLE) is a chronic, multi-system autoimmune disease. It involves the body mistakenly producing autoantibodies that attack healthy tissues and organs, including the skin.
Reader Takeaway: Seek Expert Diagnosis
Misdiagnosing lupus skin lesions as severe acne can lead to dangerous delays in treating the underlying systemic disease, potentially resulting in organ damage. Conversely, misdiagnosing common acne as lupus causes unnecessary stress and inappropriate treatment. Therefore, if a rash is persistent, accompanied by systemic symptoms (like joint pain or fever), or fails to respond to standard acne treatment, it is vital to consult a specialist, such as a Dermatologist or a Rheumatologist, for an accurate diagnosis.
Table of Contents
2. 🔬 Acne Vulgaris: Pathophysiology and Clinical Presentation
Definition: A Disorder of the Pilosebaceous Unit
Acne Vulgaris is defined as a chronic inflammatory disorder of the sebaceous glands and hair follicles. While often associated with adolescence, it can affect adults and is characterized by a range of skin lesions primarily on the face and upper trunk.
Pathophysiology: The Four Key Factors
Understanding the disease’s pathophysiology is key to effective treatment. Acne develops through a confluence of four main mechanisms:
- Sebum Overproduction: Androgen hormones stimulate the sebaceous glands to produce excessive amounts of oily sebum.
- Follicular Hyperkeratinization: Dead skin cells stick together and clog the hair follicle, trapping the sebum.
- $P$. acnes Colonization: The bacterium Propionibacterium acnes (now often called Cutibacterium acnes) thrives in the trapped sebum, multiplying rapidly.
- Inflammation: The body’s immune response to the bacteria and the ruptured follicle wall leads to visible inflammation and redness.
Common Lesions and Location
The clinical presentation of acne is diverse, classified by the type of comedones and inflammatory lesions present:
- Non-Inflammatory:
- Blackheads (Open comedones): Sebum and keratin oxidized by air.
- Whiteheads (Closed comedones): Trapped sebum under the skin’s surface.
- Inflammatory:
- Papules and Pustules: The typical “pimple” caused by mild to moderate inflammation.
- Nodules and Cysts: Severe forms involving deep, painful lesions that can lead to scarring.
Location: Acne lesions are typically confined to areas with a high concentration of sebaceous glands, mainly the face, chest, shoulders, and back.
Triggers and Risk Factors
While acne is highly prevalent, certain factors can exacerbate it: hormones (especially during puberty or menstrual cycles), specific dietary factors (high glycemic index foods, dairy), and genetics (a family history often increases risk).
3. 🛡️ Lupus Skin Lesions: Pathophysiology and Clinical Presentation
Definition: A Systemic Autoimmune Disease
Unlike localized acne vulgaris, Lupus (most commonly Systemic Lupus Erythematosus or SLE) is a chronic, body-wide autoimmune disease. In SLE, the immune system is dysregulated, producing specific autoantibodies that target the body’s own healthy cells and tissues. This misguided attack leads to widespread inflammation and potential damage across multiple organ systems.
Pathophysiology of Lupus-Related Rashes
The visible skin manifestations of Lupus are driven by this underlying autoimmune disease process. Key to the pathophysiology is the formation of immune complexes (a combination of autoantibodies, like ANA or Antinuclear Antibodies, and antigens) that deposit in the skin’s blood vessel walls and basal layer. This triggers a destructive inflammatory response.
The Signature Malar Rash
The most recognizable and concerning skin lesion associated with SLE is the Malar rash, often popularly termed the “butterfly rash.”
- Appearance and Texture: It is typically a fixed, flat (macular) or slightly raised (papular) redness that often feels warm.
- Location: Crucially, it covers the cheeks and the bridge of the nose, sparing the nasolabial folds (the skin creases from the nose to the corners of the mouth). This specific distribution is a key element in the differential diagnosis against other facial rashes.
- Trigger: The rash is highly reactive; flares are often induced or worsened by sun exposure, a hallmark known as photosensitivity.
Other Cutaneous Lupus Manifestations
Beyond the classic rash, other forms of cutaneous lupus may present:
- Discoid Lupus Erythematosus (DLE): These are chronic, scaly, elevated, disk-shaped plaques that commonly appear on the face, scalp, and ears. DLE lesions often cause atrophy and significant scarring, which can result in permanent hair loss.
- Subacute Cutaneous Lupus: This presents as non-scarring, reddish, annular (ring-shaped) or papulosquamous (scaly, raised) lesions on sun-exposed areas.
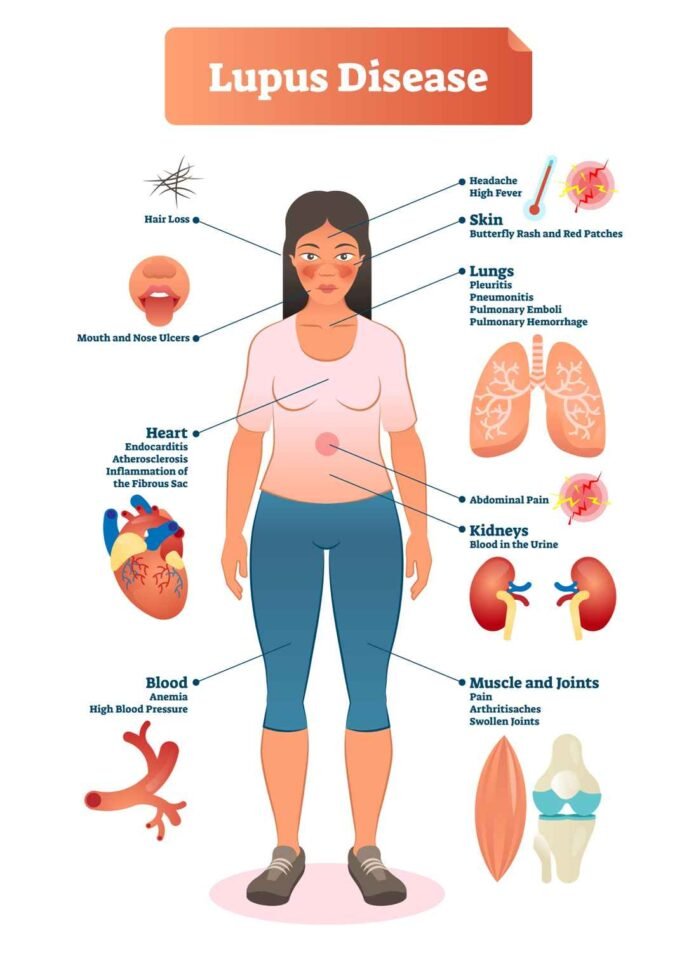
Recognizing Systemic Symptoms
A central indicator that distinguishes SLE from simple acne is the presence of systemic symptoms. Because Lupus affects the entire body, the clinical presentation goes far beyond the skin. The persistence of any of these signs alongside a suspicious rash warrants urgent medical investigation:
- Musculoskeletal: Persistent joint pain and stiffness (arthritis).
- Constitutional: Unexplained fever, overwhelming fatigue, and weight loss.
- Organ Involvement: Pleuritis (chest pain), neurological symptoms, and inflammation of the kidneys (lupus nephritis), requiring complex management by a Rheumatologist.
4. 📋 Key Differences: The Diagnostic Checklist
To facilitate rapid clinical assessment and aid the reader’s understanding of the differential diagnosis, here is a summary of the most important distinctions between acne vulgaris and Systemic Lupus Erythematosus (SLE).
Diagnostic Checklist
| Feature | Acne Vulgaris | Systemic Lupus Erythematosus (SLE) |
|---|---|---|
| Etiology (Cause) | Follicular disorder, $P$. acnes, excess sebum, and bacterial colonization. | Autoimmune disease leading to widespread inflammation and tissue damage. |
| Primary Lesions | Comedones (whiteheads, blackheads), papules, pustules, and deep cysts. | Malar rash (butterfly rash), Discoid Lupus Erythematosus (DLE) plaques, and non-scarring rashes. |
| Lesion Location | Areas with high sebaceous gland concentration (face, chest, back). | Sun-exposed areas; the Malar rash classically sparing nasolabial folds. |
| Systemic Symptoms | None. Condition is purely dermatological. | Common (persistent joint pain, profound fatigue, unexplained fever, potential organ involvement). |
| Sunlight Effect | Varies, can sometimes worsen breakouts. | Strong photosensitivity; rash and systemic symptoms frequently flare with sun exposure. |
| Diagnostic Test | Clinical examination of skin lesions; rarely requires a biopsy. | Blood tests (ANA and other autoantibodies), meeting at least four ACR criteria, sometimes a diagnostic skin biopsy (for histopathology) |
Here are the final two sections for your expert article, completing the discussion on treatment approaches and concluding with strong, authoritative advice.
5. 💊 Treatment Approaches: Tailoring Therapy to the Underlying Cause
The significant difference in pathophysiology between acne vulgaris and Systemic Lupus Erythematosus (SLE) mandates entirely different treatment strategies. Using acne medication for lupus lesions or vice versa is ineffective and can be harmful, underscoring the necessity of a correct differential diagnosis.
Acne Treatment: Targeting the Pilosebaceous Unit
Acne treatments are focused on managing sebum production, preventing follicular blockage, and reducing $P$. acnes bacteria and inflammation.
- Topical Therapies:
- Benzoyl Peroxide: Targets $P$. acnes and has a mild comedolytic effect.
- Topical Retinoids: Derivatives of Vitamin A (e.g., Tretinoin) are crucial for normalizing cell shedding and preventing the formation of comedones (clogged pores).
- Systemic Therapies:
- Oral Antibiotics: Drugs like Tetracycline or Doxycycline are used to control severe inflammation and bacterial proliferation for short periods.
- Isotretinoin: Reserved for severe, scarring, or recalcitrant acne (nodules and cysts). It dramatically reduces sebum production and is highly effective but requires rigorous monitoring.
Lupus Treatment: Controlling Systemic Autoimmunity
Lupus treatment aims to suppress the immune system’s attack, control inflammation, and prevent organ damage.
- Non-Pharmacologic Management: Strict sun protection is essential, as photosensitivity is a major trigger for rash flares (especially the Malar rash) and systemic symptoms.
- Corticosteroids:
- Topical Corticosteroids: Used to reduce local inflammation and activity in skin lesions, especially in Discoid Lupus Erythematosus (DLE).
- Systemic Corticosteroids: Used in moderate to severe SLE flares to rapidly suppress inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs):
- Hydrochloroquine (Plaquenil): Often the first-line systemic treatment for SLE and cutaneous lupus due to its anti-inflammatory and immunomodulatory effects.
- Immunosuppressants: For severe cases or those with organ-threatening involvement (e.g., lupus nephritis), powerful immunosuppressants or biologics may be required to dampen the autoimmune disease activity.
6. ✅ Conclusion: Seeking Medical Expertise
Summary: Key Telltale Signs
In summary, differentiating between the common dermatological condition of acne vulgaris and the serious autoimmune disease of Systemic Lupus Erythematosus (SLE) hinges on recognizing two major red flags:
- Lesion Type: The definitive presence of comedones (blackheads, whiteheads) strongly suggests acne. Conversely, a persistent, scarring plaque (like DLE), or the classic butterfly rash (sparing the nasolabial folds) is highly suggestive of lupus.
- Systemic Involvement: The lack of systemic symptoms (like joint pain, fever, or profound fatigue) points toward simple acne, whereas their presence necessitates testing for autoantibodies (ANA) and meeting the ACR criteria for SLE.
Actionable Advice: The Need for Accurate Diagnosis
Health decisions are YMYL (Your Money or Your Life) matters, and self-diagnosis is not an acceptable path for systemic illness. If you or a loved one exhibit a skin rash that is persistent, fails to respond to standard acne therapies, or is accompanied by other non-skin symptoms, it is absolutely crucial to seek professional medical advice.
An accurate differential diagnosis by a qualified Dermatologist or Rheumatologist ensures you receive the correct, evidence-based treatment—whether that is simple topical retinoids for acne or systemic immunosuppressants for lupus—protecting both your skin and your internal health.
Read Also:
SRS Facial: A Clear, Step-by-Step Guide to Needle-Free Skin Rejuvenation
The Ultimate Guide to Skin System Cosmetics for Beautiful and Healthy Skin