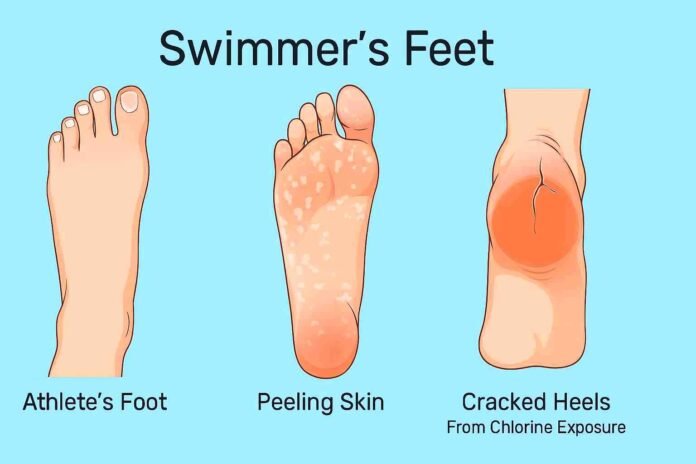
Swimmers feet is a common term used to describe a variety of foot problems that occur in people who spend a lot of time in swimming pools, locker rooms, and other damp environments. It usually refers to fungal infections like athlete’s foot, cracked heels from chlorine exposure, and skin irritation caused by prolonged moisture. In short, swimmer’s feet is a condition where the feet become itchy, flaky, dry, or infected because of constant contact with water, chemicals, and communal wet areas.
Table of Contents
What Causes Swimmer’s Feet?
The main reason behind swimmer’s feet is the combination of moisture, heat, and chemicals. When feet stay damp for long periods, fungi and bacteria thrive, especially in the areas between the toes. This often leads to athlete’s foot, a contagious fungal infection medically known as tinea pedis. Pools and locker rooms are hotspots for fungi and viruses, which is why many swimmers end up with plantar warts or peeling skin after regular exposure.
Chlorine, although important for disinfecting pools, strips the skin of its natural oils. This leaves the feet vulnerable to dryness, cracking, and irritation, especially around the heels. On top of that, walking barefoot in public areas increases the risk of catching infections since these surfaces are rarely free of microorganisms. In some cases, poor foot hygiene, such as not drying feet properly, reusing wet socks, or wearing tight shoes, worsens the problem and makes swimmers feet harder to control.
Symptoms of Swimmers Feet
The symptoms of swimmer’s feet vary, depending on whether the problem is fungal, bacterial, or chemical-related, but they all cause discomfort. The most common sign is itching and burning, especially between the toes, which is characteristic of athlete’s foot. Alongside this, many swimmers notice redness, flaking, and peeling skin that may even form small blisters. Prolonged exposure to chlorine often results in dry, cracked heels, which can sometimes bleed or become painful. In more serious cases, the cracks allow bacteria to enter, leading to infections that require medical care.
Some swimmers also develop plantar warts, which are small growths on the soles of the feet caused by the human papillomavirus (HPV). Pain while walking, persistent odor, and increased skin sensitivity are additional signs that swimmers feet may be present. Recognizing these symptoms early is important because fungal and bacterial infections spread quickly if not treated.
Treatment Options for Swimmer’s Feet
Treating swimmer’s feet depends on addressing both the infection and the dryness. For fungal infections like athlete’s foot, antifungal creams, sprays, and powders available over the counter are usually effective. These medications should be applied consistently, even after symptoms improve, to prevent recurrence. To deal with dryness and cracked heels, thick moisturizers or heel balms containing urea or shea butter are recommended, as they restore hydration and strengthen the skin barrier.
Natural remedies such as soaking feet in warm water with Epsom salt or apple cider vinegar can help reduce odor, fight bacteria, and soothe irritation. Keeping feet clean and dry is a simple yet powerful treatment step, as fungi cannot thrive without moisture.
In cases where swimmers feet causes severe infections, pain, or plantar warts, consulting a podiatrist or dermatologist becomes necessary. Doctors may prescribe stronger antifungal drugs, antibiotics, or even minor procedures to remove warts.
Preventing Swimmers Feet
The best way to manage swimmer’s feet is prevention, since once an infection develops, it can take weeks to fully clear. Always wear flip-flops or shower shoes in locker rooms, public pools, and shared showers to reduce contact with contaminated surfaces. After swimming or bathing, thoroughly dry your feet, especially between the toes, as this is where fungus usually begins. Applying antifungal powder before wearing socks can keep feet dry and protected, while moisturizing daily helps combat chlorine-induced dryness and prevents cracked heels.
Changing socks and shoes frequently ensures that moisture does not build up, reducing the chances of fungal growth. Pool shoes, sandals, and flip-flops should also be cleaned regularly, as fungi and bacteria can linger on them. Good hygiene, combined with protective habits, is the most effective shield against swimmers feet.
Final Thoughts
Swimmer’s feet may not sound serious at first, but it can quickly turn into a persistent and painful condition if ignored. The combination of fungal infections like athlete’s foot, cracked heels from chlorine, and irritation from moisture makes it both uncomfortable and unattractive. Fortunately, with proper treatment and consistent prevention, you can avoid most of the common problems associated with swimmers feet.
If symptoms don’t improve with home care, seeking medical attention ensures that the condition is treated effectively before it spreads further. Healthy feet are not only important for swimmers but for everyone who values comfort, mobility, and long-term skin health.
FAQs About Swimmer’s Feet
1. Is swimmers feet the same as athlete’s foot?
Swimmer’s feet and athlete’s foot are related, but they are not exactly the same thing. Athlete’s foot (tinea pedis) is a fungal infection caused by dermatophytes that thrive in warm, moist environments such as swimming pools, locker rooms, and communal showers. On the other hand, swimmer feet is a broader term that describes various foot problems swimmers face, including fungal infections, cracked heels, chlorine irritation, and plantar warts. In most cases, swimmer’s feet includes athlete’s foot, but it also covers other skin issues caused by water and chemical exposure.
2. How do you treat cracked heels from swimming?
Cracked heels are one of the most common symptoms of swimmer feet, especially for people who swim regularly in chlorinated pools. Chlorine strips the skin of its natural oils, making it dry and prone to cracking. To treat cracked heels, it’s best to apply a thick heel balm or moisturizer containing urea, shea butter, or coconut oil after swimming. Wearing cotton socks overnight after moisturizing helps lock in hydration. For severe cracks, soaking feet in Epsom salt water or gently exfoliating with a pumice stone can speed up healing. Keeping the heels moisturized and protected prevents deeper fissures that can lead to infection.
3. Can plantar warts be part of swimmer’s feet?
Yes, plantar warts are often considered a part of swimmers feet because they are commonly contracted in the same environments. Plantar warts are caused by the human papillomavirus (HPV), which spreads easily in damp areas like public pools and showers. Unlike fungal infections, plantar warts appear as small, rough growths on the soles of the feet and may cause pain when walking. Treatment options include over-the-counter wart removal solutions, salicylic acid patches, cryotherapy (freezing by a doctor), or laser treatment. Wearing flip-flops in communal areas and disinfecting footwear are effective ways to prevent plantar warts from developing in the first place.
4. How long does it take to heal swimmers feet?
The healing time for swimmers feet depends on the severity of the condition and the type of problem involved. Mild cases of athlete’s foot usually improve within two to four weeks when treated with antifungal creams or sprays. Cracked heels may take a few days to weeks to recover, depending on how deep the cracks are and how consistently moisturizers are applied. Plantar warts, however, can take several weeks or even months to disappear, as they require stronger treatment or medical removal. The key to faster healing is combining treatment with good foot hygiene and prevention practices, so the infection or irritation doesn’t return.
5. How can swimmers prevent fungal foot infections?
Preventing fungal infections is easier than treating them, and it’s the most important step for anyone prone to swimmers feet. Swimmers should always wear shower shoes or flip-flops in locker rooms, public pools, and showers to avoid direct contact with fungi and bacteria. After swimming, feet should be dried thoroughly, especially between the toes, since damp areas encourage fungal growth. Applying an antifungal powder or spray before putting on socks or shoes helps keep feet dry and protected. Moisturizing after swimming protects against chlorine-induced dryness and cracking, while regularly disinfecting pool sandals and washing socks in hot water ensures fungi don’t linger on fabrics.
Read Also: